45 Overweight and Underweight—What are the Risks?
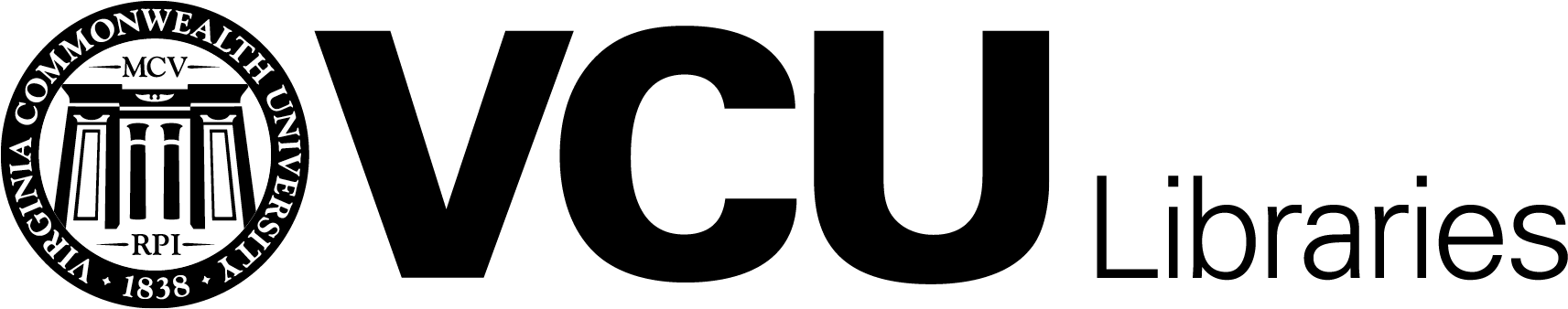
As the previous section illustrated, energy balance is influenced by many factors. Whether an individual is in positive or negative energy balance ultimately influences the overall trend in whether that individual is normal weight, overweight, or underweight. While much of the focus in society is placed on concerns with being overweight or obese, both ends of the weight spectrum are associated with health risks, and being underweight can negatively impact health just as being overweight can. In fact, research has shown a J-shaped association between mortality risk and BMI, with greater risk for dying in underweight and obese populations and the lowest risk occuring in the normal BMI range.1
Figure 7.14. The relationship between body mass index and mortality forms a J-shaped curve, demonstrating higher rates of death associated with underweight and overweight/obese, with lowest rates of death associated with normal weight.
What are the specific risks associated with being overweight or underweight? Let’s take a closer look at each of these situations.
Health Risks of Being Overweight or Obese
The health consequences of too much body fat are numerous. Fat cells are not lifeless storage tanks—they’re dynamic, metabolically-active tissue that secrete a number of different hormones and hormone-like messengers, causing low-grade inflammation that’s believed to contribute to chronic disease development such as type 2 diabetes, cardiovascular disease, and some types of cancer.
According to the World Health Organization (WHO), there are more people worldwide who are overweight or obese than underweight, and an estimated 2.8 million adults die annually as a result of being overweight or obese.2 As BMI increases over 25, the risks increase for several health conditions,3 including:
- Heart disease
- Type 2 diabetes
- Hypertension
- Stroke
- Osteoarthritis
- Sleep apnea
- Some cancers (endometrial, breast, colon, kidney, gallbladder, liver)
- Depression and anxiety
- Difficulty with physical movement
- Lower quality of life
Childhood obesity is also a global health concern. In 2016 over 340 million children and adolescents and 41 million preschool children were overweight or obese. And obese children are more likely to become obese adults, develop diabetes and cardiovascular disease at younger ages, and have an increased risk of premature death.2
Similar to other public health organizations, the WHO states that the main causes of the global obesity epidemic are increased intake of energy-dense foods and decreased physical activity associated with modernization, industrialization, and urbanization. The environmental changes that contribute to the dietary and physical activity patterns of the world today are associated with the lack of policies that address the obesity epidemic in the food and health industry, urban planning, agriculture, and education sectors.2
Economic and Societal Costs of Being Overweight and Obese
The economic burden of overweight and obesity has skyrocketed as obesity rates in the United States continue to climb. According to a recent report, direct health care costs due to overweight and obesity (money directly paid to treat the illness) exceed $480 billion and indirect health care costs (lost economic productivity due to absenteeism, lost wages, and reduced productivity) have surpassed $1.2 trillion.4 On the individual level, people who are obese spend $3,429 more per year for medical care than people of healthy weight.5
Social and emotional consequences of being overweight or obese are no less real than economic costs. Individuals with obesity often face discrimination, lower wages, depression, anxiety, and lower quality of life.3,6 Weight bias and discrimination are of particular concern for those who are overweight or obese. Weight bias is defined as “negative weight-related attitudes, beliefs, assumptions and judgments toward individuals who are overweight and obese,” though this bias does extend to those who are underweight as well.7
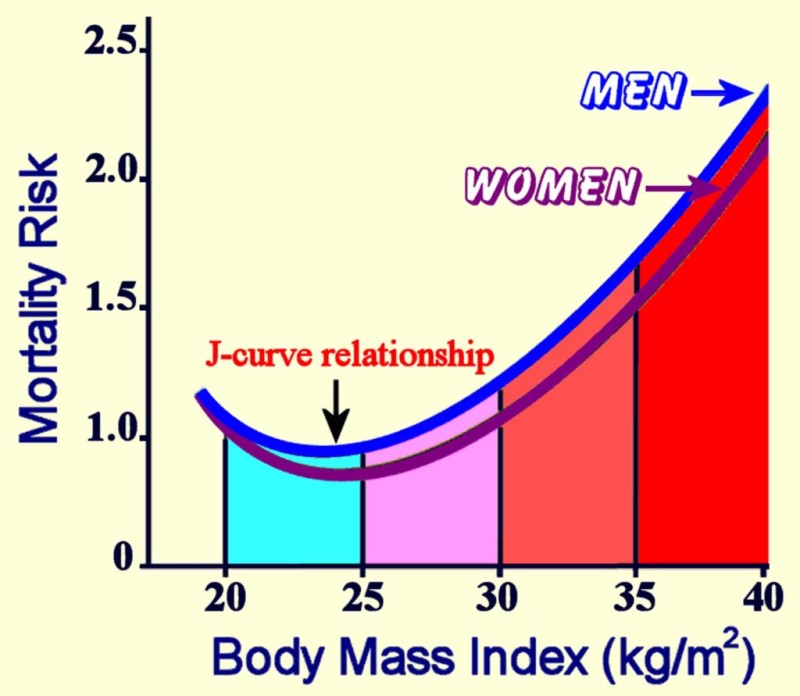
Incidence of weight discrimination has increased by 66 percent since 1995 and occurs at rates similar to that of racial discrimination.8 According to Rebecca Puhl, PhD, deputy director of the Rudd Center for Food Policy & Obesity at the University of Connecticut, “Bias, stigma, and discrimination due to weight are frequent experiences for many individuals with obesity, which have serious consequences for their personal and social well being and overall health.”9 Puhl has also noted that “about 40% of the general population reports that it has experienced some type of weight stigma—whether it be weight-based teasing, unfair treatment, or discrimination.”10 Individuals who are obese are often blamed for their disease and viewed as being lazy, stupid, ugly, and lacking in self-control or motivation.11 This bias toward people with obesity is seen in many aspects of life, including the workplace, health care, social environments, and even the individual’s own family.
Figure 7.15. Common sources of weight stigmatization identified by individuals who are overweight or obese include families, social environments, work environments, and service providers, as well as generalized feelings of judgment from others. Source: Cossrow, N. H., Jeffery, R. W., & McGuire, M. T. (2001). Understanding weight stigmatization: A focus group study. Journal of nutrition education, 33(4), 208-214.
Combatting weight bias and discrimination will require change on many levels. Governments can include weight as a category covered in anti-discrimination laws. Anti-bullying efforts at the school level should include policies on harassment and bullying related to weight. Health care should include reimbursement for obesity treatment, and weight bias training should be required for health care providers. And education and awareness about weight bias on an individual level will help change negative attitudes toward overweight and obesity.9,12
Video: “Weight of the Nation: Stigma—The Human Cost of Obesity” by HBO Docs, YouTube (May 14, 2012), 18:54. This is an excellent video to help increase awareness of weight stigma, humanizing the pain and damage caused by weight bias and discrimination.
Health Risks of Being Underweight
The 2015–2016 National Health and Nutrition Examination Survey (NHANES) estimated that 1.5 percent of adults and 3.0 percent of children and adolescents in the United States are underweight.13,14 Underweight individuals represent a small portion of Americans, yet the health risks associated with being underweight are an important part of the discussion on nutrition and health.
Being underweight is linked to nutritional deficiencies, especially iron-deficiency anemia, and to other problems such as delayed wound healing, hormonal abnormalities, increased susceptibility to infection, and increased risk of some chronic diseases such as osteoporosis. In children, being underweight can stunt growth. The most common underlying cause of underweight in America is inadequate nutrition. Other causes are wasting diseases (cancer, multiple sclerosis, tuberculosis) and eating disorders. People with wasting diseases are encouraged to seek nutritional counseling, as a healthy diet greatly affects survival and improves responses to disease treatments.
Eating Disorders
The National Institute of Mental Health (NIMH) defines eating disorders as “serious and sometimes fatal illnesses that cause severe disturbances to a person’s eating behaviors.”15 People with eating disorders often experience a preoccupation with food choices and body weight, and they frequently have a distorted body image, believing that self-worth is tied to body size and shape.16
Eating disorders that result in underweight affect about eight million Americans (seven million women and one million men). And eating disorders have the second highest mortality rate of mental illnesses, outranked only by opioid addiction.17 Prevention and proper treatment of eating disorders must involve a multi-faceted approach, including physical, emotional, and social issues related to each individual’s needs.18
Anorexia Nervosa
Anorexia nervosa, more often referred to as “anorexia,” is a psychiatric illness in which a person obsesses about their weight and about the food that they eat. Anorexia results in extreme nutrient inadequacy and eventually organ malfunction. Anorexia is relatively rare—the NIMH reports that 0.9 percent of females and 0.3 percent of males will have anorexia at some point in their lifetime, but it is an extreme example of how an unbalanced diet can affect health.15
Anorexia frequently manifests during adolescence, although it may emerge much later in adulthood as well. People with anorexia consume, on average, fewer than 1,000 calories per day and exercise excessively. They are in a tremendous caloric imbalance. Moreover, some may participate in binge eating, self-induced vomiting, and purging with laxatives or enemas. The exact causes of anorexia are not completely known, but many things contribute to its development including economic status, as it is most prevalent in high-income families. It is a genetic disease and is often passed from one generation to the next. Complications during fetal development and abnormalities in the brain, endocrine system, and immune system may all contribute to the development of this illness.
The primary signs of anorexia are fear of being overweight, extreme dieting, an unusual perception of body image, and depression. The secondary signs and symptoms of anorexia are all related to the caloric and nutrient deficiencies of the unbalanced diet and include excessive weight loss, a multitude of skin abnormalities, diarrhea, cavities and tooth loss, osteoporosis, and liver, kidney, and heart failure. There is no physical test that can be used to diagnose anorexia and distinguish it from other mental illnesses. Therefore, a correct diagnosis involves eliminating other mental illnesses, hormonal imbalances, and nervous system abnormalities. Treatment of any mental illness involves not only the individual, but also family, friends, and a psychiatric counselor. Treating anorexia often involves a registered dietitian, who helps to provide dietary solutions that are adjusted over time. The goals of treatment for anorexia are to restore a healthy body weight and significantly reduce the weight obsession and behaviors associated with the eating disorder. Relapse to an unbalanced diet is high. Many people do recover from anorexia; however, most continue to have a lower-than-normal body weight for the rest of their lives.
Bulimia
Bulimia, like anorexia, is a psychiatric illness that can have severe health consequences. The NIMH reports that 0.5 percent of females and 0.1 percent of males will have bulimia at some point in their lifetime.15
Bulimia is characterized by episodes of eating large amounts of food followed by purging, which is accomplished by vomiting and with the use of laxatives and diuretics. Unlike people with anorexia, those with bulimia often have a normal weight, making the disorder more difficult to detect and diagnose. Bulimia is characterized by signs similar to anorexia such as fear of being overweight, extreme dieting, and bouts of excessive exercise. Secondary signs and symptoms include gastric reflux, severe erosion of tooth enamel, dehydration, electrolyte imbalances, lacerations in the mouth from vomiting, and peptic ulcers. Repeated damage to the esophagus puts people with bulimia at an increased risk for esophageal cancer. The disorder is also highly genetic, linked to depression and anxiety disorders, and most commonly occurs in adolescent girls and young women. Treatment often involves antidepressant medications and, like anorexia, has better results when both the family and the individual with the disorder participate in nutritional and psychiatric counseling.
Figure 7.16. This photo shows the erosion on the lower teeth caused by bulimia. For comparison, the upper teeth were restored with porcelain veneers.
Binge-Eating Disorder
Similar to those who experience anorexia and bulimia, people with binge-eating disorder have lost control over their eating. Binge-eating disorder was only recently classified as a distinct psychiatric illness, becoming formally recognized as a diagnosable eating disorder in 2013. People with binge-eating disorder will periodically overeat to the extreme, but their loss of control over eating is not followed by fasting, purging, or compulsive exercise. As a result, people with this disorder are often overweight or obese, and their chronic disease risks are those linked to having an abnormally high body weight such as hypertension, cardiovascular disease, and Type 2 diabetes. Additionally, they often experience guilt, shame, and depression. Binge-eating disorder is commonly associated with depression and anxiety disorders. According to the NIMH, binge-eating disorder is more prevalent than anorexia and bulimia, and affects almost 3 percent of individuals at some point during their lifetime.15 Treatment often involves antidepressant medication as well as nutritional and psychiatric counseling.
Orthorexia
Orthorexia is a newer disordered eating behavior defined as an obsession with healthy eating. The term “orthorexia” was first defined in 1998, but it has yet to be formally classified as an eating disorder, making it difficult to determine how prevalent it is. Research suggests it may be identified as a form of obsessive-compulsive disorder.19 While focusing on a healthy diet isn’t inherently a bad thing, in situations of orthorexia, the individual takes the emphasis of healthy eating, or “clean” eating, to the extreme, so much so that it becomes a fixation, putting their health at risk.19
Signs of orthorexia include compulsively reading food labels, cutting several food groups out of the diet, spending an unusual amount of time focusing on what foods may be available at upcoming events, and experiencing a high level of stress when healthy foods are not available. The obsession with healthfulness comes with a high social cost as it is often difficult to enjoy eating out or sharing meals with friends and family.
There is no formal treatment plan for orthorexia, but many eating disorder experts treat it similarly to anorexia and obsessive-compulsive disorder.19
If you think you or someone close to you might have an eating disorder and you want to learn more or find resources for help, check out these organizations and links.
https://www.nationaleatingdisorders.org/help-support
https://anad.org/our-services/eating-disorders-helpline/
https://www.eatingdisorderhope.com/
Self-Check
Attributions:
- University of Hawai‘i at Mānoa Food Science and Human Nutrition Program, “Undernutrition, Overnutrition, and Malnutrition,” CC BY-NC 4.0
References:
- 1Di Angelantonio, E., Bhupathiraju, S. N., Wormser, D., Gao, P., Kaptoge, S., de Gonzalez, A. B., … & Lewington, S. (2016). Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet, 388(10046), 776-786.
- 2Obesity and overweight. (2017). World Health Organization. Retrieved October 31, 2019 from https://www.who.int/features/factfiles/obesity/en/.
- 3The health effects of overweight and obesity. (2015). Centers for Disease Control and Prevention. Retrieved October 31, 2019, fromhttps://www.cdc.gov/healthyweight/effects/index.html.
- 4Economic impact of excess weight. (2018). Milken Institute. Retrieved November 4, 2019, from https://milkeninstitute.org/articles/economic-impact-excess-weight-now-exceeds-17-trillion-new-milken-institute-report-reveals.
- 5Obesity. America’s health rankings. Retrieved October 31, 2019, from https://www.americashealthrankings.org/explore/annual/measure/Obesity/state/OR.
- 6Obesity consequences. Harvard T.H. Chan School of Public Health. Retrieved November 4, 2019, from https://www.hsph.harvard.edu/obesity-prevention-source/obesity-consequences/economic/.
- 7Alberga, A. S., Russell-Mayhew, S., von Ranson, K. M., & McLaren, L. (2016). Weight bias: a call to action. Journal of eating disorders, 4(1), 34.
- 8Schvey, N. (2010). Weight bias in health care. AMA Journal of Ethics. Retrieved November 7, 2019, from https://journalofethics.ama-assn.org/article/weight-bias-health-care/2010-04.
- 9Understanding obesity stigma. (2019). Obesity Action Coalition. Retrieved November 7, 2019, from https://www.obesityaction.org/get-educated/public-resources/brochures-guides/understanding-obesity-stigma-brochure/.
- 10Blog, R. L., & by Age, N. The Health Impact of Weight Stigma By Carrie Dennett, MPH, RDN, CD Today’s Dietitian Vol. 20, No. 1, P. 24. Retrieved November 7, 2019, from
https://www.todaysdietitian.com/newarchives/0118p24.shtml. - 11Swinburn, B. A., Kraak, V. I., Allender, S., Atkins, V. J., Baker, P. I., Bogard, J. R., … & Ezzati, M. (2019). The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. The Lancet, 393(10173), 791-846.
- 12Weight bias: A social justice issue. UConn Rudd Center for Food Policy & Obesity. Retrieved November 4, 2019, from http://www.uconnruddcenter.org/policy-briefs-and-reports.
- 13Prevalence of underweight among adults aged 20 and over: United States, 1960–1962 through 2015–2016. (2018). Centers for Disease Control and Prevention. Retrieved November 4, 2019, from https://www.cdc.gov/nchs/data/hestat/underweight_adult_15_16/underweight_adult_15_16.htm.
- 14Prevalence of underweight among children and adolescents aged 2–19 years: United States, 1963–1965 through 2015–2016. (2018). Centers for Disease Control and Prevention. Retrieved November 4, 2019, from https://www.cdc.gov/nchs/data/hestat/underweight_child_15_16/underweight_child_15_16.pdf.
- 15Eating disorders. (2017). The National Institute of Mental Health. Retrieved November 4, 2019, from https://www.nimh.nih.gov/health/statistics/eating-disorders.shtml#part_155061.
- 16Body image. (2018). National Eating Disorder Association. Retrieved November 4, 2019, from https://www.nationaleatingdisorders.org/toolkit/parent-toolkit/body-image.
- 17Statistics and research on eating disorders. (2018). National Eating Disorder Association. Retrieved November 4, 2019, from https://www.nationaleatingdisorders.org/statistics-research-eating-disorders.
- 18Prevention. (2018). National Eating Disorder Association. Retrieved November 4, 2019, from https://www.nationaleatingdisorders.org/learn/general-information/prevention.
- 19Orthorexia. (2018). National Eating Disorder Association. Retrieved November 7, 2019, from https://www.nationaleatingdisorders.org/learn/by-eating-disorder/other/orthorexia.
Image Credits:
- Figure 7.14. “Relationship Between Body Mass Index (BMI) and Mortality“ is in the Public Domain, CC0
- Figure 7.15. “Sources of Stigmatization” by Heather Leonard is licensed under CC BY 4.0
- “Stop Bullying” by jstn-1-7_pe is licensed under CC BY 2.0
- “woman on scale” by Luxstorm is licensed under CC BY 2.0
- Figure 7.16. “Oral Manifestation of Bulimia” by Jeffrey Dorfman is licensed under CC BY-SA 3.0
Negative attitudes, beliefs, assumptions and judgments toward individuals based on their body size.
An eating disorder in which a person obsesses about their weight and the food that they eat, resulting in extreme nutrient inadequacy and eventually organ malfunction.
An eating disorder characterized by episodes of eating large amounts of food followed by purging, which is accomplished by vomiting and with the use of laxatives and diuretics.
An eating disorder characterized by periodic overeating with a feeling of loss of control over eating but not accompanied with fasting, purging, or compulsive exercise.
An extreme, unhealthy fixation on healthy or “clean” eating.